By Donna Motley, Vice President of Claims
HOW TO FILE A CLAIM – Sounds simple, right? There is more involved than one might anticipate.
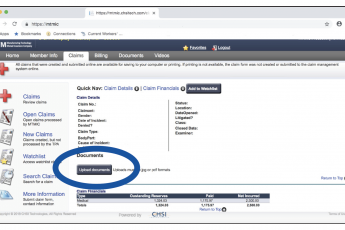
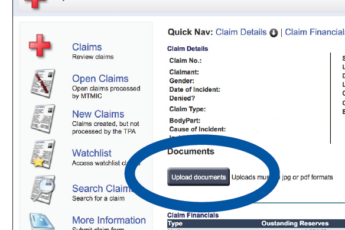
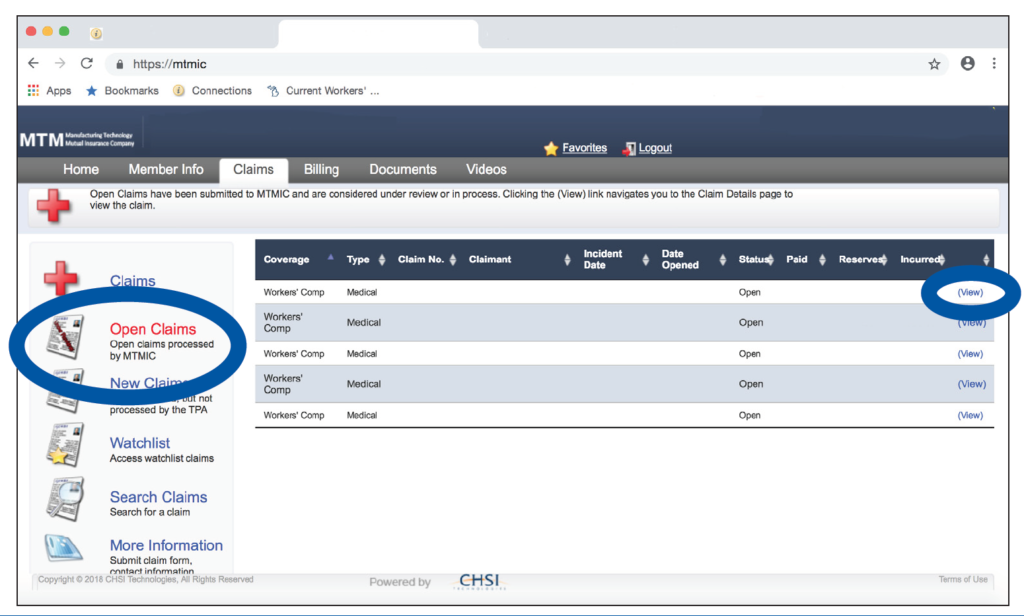
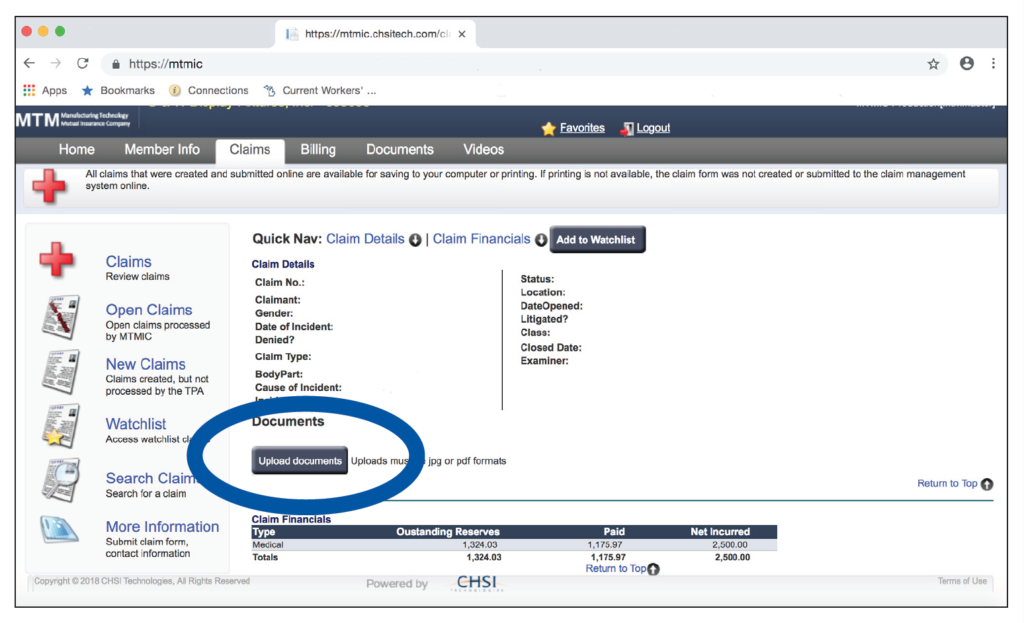
Claims can be filed with our department via facsimile, e-mail or MTMIC’s Portal. (No one uses U.S. mail anymore – if for no other reason, it takes too long!) Early reporting is best. The longer the delay between the date of injury and the date received in our office results in additional investigation of the circumstances surrounding the incident. Causal relationship has to be identified. When claims are reported within one or two days of occurrence, most, if not all, details are still fresh in everyone’s mind. Similar to the childhood game of “re-telling” a story, the more time that passes, the more likely the story (or in this case, facts) can change. Studies have been done where five people witness the same motor vehicle accident, and there are five different versions as to “how” the accident occurred. Wait an additional five days and details tend to blur, change or be forgotten.
(more…)